Diverticular Disease
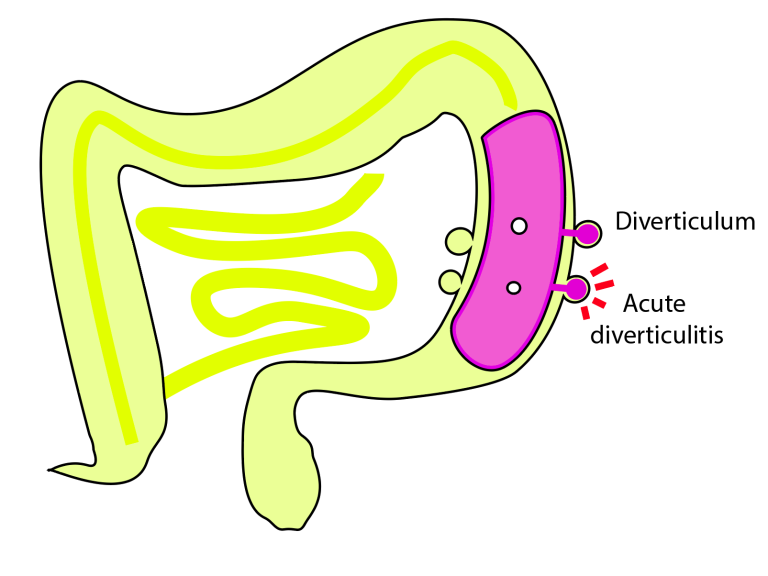
Diverticular disease is a “wear and tear” problem of the large bowel (colon). Small pouches form in areas of weakness of the wall of the bowel.
This can cause problems when they become inflamed or infected (diverticulitis).
We don’t know why some people get this problem and some don’t. It is more common with age, as the bowel wall becomes more stretchy and floppy.
How is it diagnosed?
It can be seen on CT scans, and at colonoscopy.
What problems can it cause?
It is important to remember that most people with diverticular disease will never have any complications, and can carry on with their lives as normal.
The most common symptoms include:
- Lower abdominal pain
- Bloating
- Change in bowel habit
- Mucus or blood in the stool
The pattern of symptoms differs from one person to the next, but pain is often crampy, and left sided. Pain and bloating can often start after food is eaten, and may ease after passing wind or stool.
Complications
Relatively few people ever get symptoms severe enough for them to be admitted to hospital. However complications can occur and these include:
- Inflammation (diverticulitis)
This is the most common complication, affecting 1 in 10 people with the condition. It causes worsening abdominal pain, fever, and diarrhoea. This is normally treated with antibiotics and plenty of oral fluids
- Perforation
The bowel wall of a diverticulum is thin, and when inflamed can perforate. This lets bowel content into the abdomen and causes sepsis. This requires admission hospital for intravenous antibiotics. A small proportion may require emergency surgery.
- Bowel blockage
Repeated episodes of inflammation can cause scar tissue around the iflammed diverticulum. Over time this can narrow the bowel, making it hard for stool to pass.
- Bleeding
A blood vessel in the thin walled divertulum can rupture, causing large volume fresh rectal bleeding. This may seal up by itself, or may require admission to hospital to help stop the bleeding. It may require a blood transfusion.
- Fistula
Rarely, persistent inflammation related to diverticular disease can create abnormal connections from the bowel to other organs (eg. bladder, vagina). If diagnosed, then an operation can usually fix this.
What can I do to live well with diverticular disease?
Most people with diverticular disease learn to live with it.
- Diet
A healthy diet is advised, eating plenty of fibre. A good water intake (1+ litre fluid a day) will help the fibre to pass through the gut. There is no need to avoid seeds, nuts, or fruit skins.
- Exercise
You should take regular exercise, watch your weight, and refrain from smoking.
- Medicines
There is no medicinal cure for diverticular disease. A bulk forming laxative such as fybogel can help to avoid constipation, if that is a problem for you.
- Surgery
This is usually a treatment of last resort, as complication rates are high. An operation would normally remove the affected part of the bowel, and can often necessitate a temporary stoma (end of the bowel brought to the surface of the skin).
Further sources of information
©Copyright. All rights reserved.
We need your consent to load the translations
We use a third-party service to translate the website content that may collect data about your activity. Please review the details in the privacy policy and accept the service to view the translations.